Patella dislocation is a common problem seen in young athletic persons. Non-operative treatment is usually adviced for the first episode of dislocation. Adequate rest followed by muscle strengthening help in recover of this problem.
This dislocation of the patella from its groove (trochlear groove) can occur due to a blow to the inner aspect of the knee joint or due to violent contraction of the thigh muscle which can pull the patella out of it normal position in the trochlear groove.
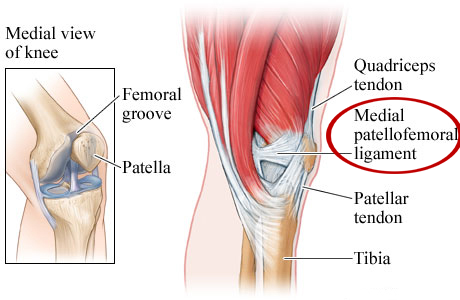
If the patella has dislocated more than once, we have to investigate for the reason for such occurrence. There is a support for the patella on the inner aspect of the knee called Medial Patellofemoral Ligament (MPFL), which prevents the outward movement of the patella.
What causes patellar instability?
The kneecap is part of the skeletal system. Connective tissues (muscles, tendons and ligaments) in the front of the thighbone (femur) go over the kneecap and connect to the shinbone (tibia). These muscles pull the kneecap up through the trochlear groove when you straighten your leg and down the groove when you bend it. When the kneecap is unstable, it moves outside of this groove.
Causes of patellar instability include:
- Shallow or uneven trochlear groove.
- Loose ligaments or extremely flexible joints.
- Sharp blow to the kneecap during a fall, sports injury or other accident.
What is a Medial Patellofemoral Injury?
The medial patellofemoral ligament is a broad structure located on the inside of the knee joint. It connects the kneecap (patella) to the thigh bone (femur). The primary purpose of the MPFL is to provide stability to the kneecap; it provides restraint to any movement toward the outside of the knee. It also helps keep the kneecap in position, as the knee bends and straightens.

What are the risk factors for patellar instability?
Anyone can develop patellar instability. Females tend to have looser ligaments that make them more prone to patellar instability.
You may have higher risk if you play high-impact sports like football or do activities that require a lot of quick pivoting, like basketball, cheer or soccer.
How Does it Feel?
Common signs and symptoms that may occur with an MPFL injury include:
- Feeling the knee “giving way” or “buckling” during activity.
- Feeling like the kneecap is sliding out to the side during knee movement.
- Swelling of the knee following activity.
- Restricted joint movement (range of motion).
- Pain when moving the joint.
- Tenderness to touch along the affected joint.
- Pain, stiffness, or “locking,” after sitting with the knee bent or straight for a prolonged period of time
What is the link between patellar instability and a dislocated kneecap?
Patellar instability can lead to a dislocated kneecap. You may have:
- Complete dislocation: The ligaments that hold the kneecap in place slide to the outside of the knee, taking the kneecap with them. The ligaments may tear or stretch. The kneecap is entirely out of place.
- Partial dislocation (subluxation): The kneecap slips partially out of the groove.
How is patellar instability diagnosed?
Even if your kneecap moves back into place on its own, you should see your healthcare provider for a diagnosis and potential treatment. Your provider will perform a physical exam to assess symptoms, including your range of motion.
You may also get:
- X-rays to see if the kneecap is out of place and check for mal-aligned bones
- MRI scan to check for injuries like Medial patellofemoral ligament tear, anterior cruciate ligament (ACL) tears, meniscal tears and loose bone fragments.
MRI scan
MRI measurements in patellar instability
These are the measurements to be done to understand the reasons for the patella dislocation. If all the regions of the extensor mechanism with their angles and points of contact are not measured, surgical correction can fail.
What are nonsurgical treatments for patellar instability?
If the kneecap doesn’t move back to the trochlear groove on its own, seek medical attention. A healthcare provider will gently push the kneecap back into place. This process (reduction) can be uncomfortable. You may receive pain medications , but you shouldn’t need anesthesia.
For partial knee dislocations and patellar instability, you may be given:
- Knee brace to immobilize the knee and keep the kneecap in place. You may need to wear a brace for several weeks and use crutches during this time.
- Nonsteroidal anti-inflammatory drugs (NSAIDs), rest, elevation and ice packs to ease pain and swelling.
- Physical therapy to strengthen muscles that hold the kneecap in place and improve range of motion.
What are surgical treatments for patellar instability?
If you have chronic patellar instability or a complete kneecap dislocation, your healthcare provider may recommend surgery. Most knee surgeries take place arthroscopically. The procedure uses small incisions and a tiny camera (arthroscope). Recovery can take six to 12 months.
If an injury causes patellar instability, you may have loose cartilage or bone fragments in the knee. Your provider will surgically remove them.
Surgical options include:
- Medial patellofemoral ligament (MPFL) repair to strengthen and repair the ligaments that hold the kneecap in place.
- MPFL reconstruction to replace a damaged ligament with a hamstring tendon taken from a donor or elsewhere in your body.
- Knee osteotomy (tibial tubercle transfer) to realign the shinbone, thighbone, kneecap and connective tissues. This open surgical procedure requires a larger incision and longer recovery than arthroscopic surgery.
- Knee replacement to treat severe arthritis or recurrent dislocations.
How can I prevent patellar instability?
An unstable kneecap can damage connective tissue. That damage increases your risk for repeat kneecap dislocations.
Physical therapy exercises can strengthen muscles and connective tissue that keep the kneecap in the femoral groove. Cycling on an exercise bike or outside on an actual bike is also a good knee strengthener. You may be recommended to wear a knee brace during certain activities.
What is the outlook for people with patellar instability?
Nearly half of people who complete nonsurgical treatments for patellar instability will dislocate the knee again. This means the kneecap is still unstable.
Chronic patellar instability increases your risk of developing arthritis and ligament damage. Your doctor may recommend surgery.
MRI / Xray measurements before planning Surgical correction of patella instability


 Call us:+91-484 2885910 (Reception Orthopedics; 9am to 5pm Mon-Sat), +91-484-2885621 (22,23,24)
Doctor's mobile - +91 9497559755 (whatsapp only please)
Call us:+91-484 2885910 (Reception Orthopedics; 9am to 5pm Mon-Sat), +91-484-2885621 (22,23,24)
Doctor's mobile - +91 9497559755 (whatsapp only please)









